Step 1: Root Operation
As with all inpatient procedure coding, the first step is to identify the root operation or intent of the procedure. Angioplasty is performed to dilate occluded vessels, so the root operation is Dilation. The official PCS definition of Dilation is “Expanding an orifice or the lumen of a tubular body part.” Depending on whether the targeted artery is above or below the diaphragm, this will lead you to table 037 (dilation of upper arteries) or 047 (dilation of lower arteries).
Body Part
Step 2: Branch of a Body Part Without a Specific PCS Body Part Value
The second step in angioplasty is to identify the body part or specific artery that is being dilated. That may sound very straightforward until you get to an artery that does not have a body part value in PCS or an angioplasty is performed on a bridging lesion. This is where the PCS guidelines come into play.
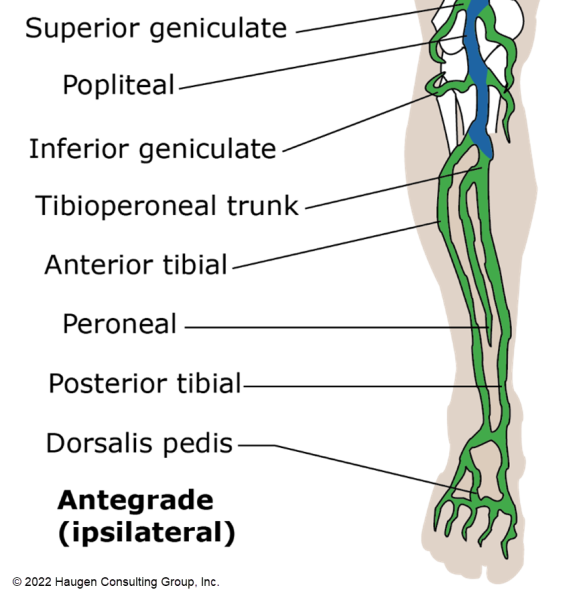
Official coding guideline (OCG) B4.2 addresses coding for a specific branch of a body part that does not have its own body part value. When this is the case, the body part located closest to the proximal branch that has a specific body part value is coded. For example, there is no body part for the right tibioperoneal trunk. The closest proximal (closest to heart) artery is the right popliteal artery; therefore, the body part for angioplasty of the right tibioperoneal trunk is the right popliteal artery.
There is an exception to this guideline, however. Should coding to the most proximal branch cause the case to code to a different body system, a general body part value is assigned. For example, the fifth intercostal artery is an upper artery (above the diaphragm), which extends from the aorta. By coding aorta as the body part, the body system changes from Upper Arteries to Heart and Great Vessels. Rather than coding to a different body system, the body part value Upper Artery (Y) is chosen from the Upper Arteries body system.

Don’t forget to use the Body Part Key if you aren’t sure which body part to select. The Body Part Key is based on the ICD-10-PCS guidelines and conventions. A good reference showing vascular anatomy is also helpful. Our VIR Flip Bits are a valuable tool for assisting in anatomy.
Step 3: Bridging Lesions
A bridging lesion is one that extends from one artery to another. OCG B4.1c addresses coding for bridging lesions and has changed a lot over the last several years. As of October 1, 2021, for fiscal year 2022, the guideline reads:
If a procedure is performed on a continuous section of a tubular body part, code the body part value corresponding to the anatomically most proximal (closest to the heart) portion of the tubular body part.
Example: A procedure performed on a continuous section of artery from the femoral artery to the external iliac artery with the point of entry at the femoral artery is coded to the external iliac body part. A procedure performed on a continuous section of artery from the femoral artery to the external iliac artery with the point of entry at the external iliac artery is also coded to the external iliac artery body part.
Occlusion of the bronchial artery is coded to the body part value Upper Artery in the body system Upper Arteries, and not to the body part value Thoracic Aorta, Descending in the body system Heart and Great Vessels.
This guideline is used frequently when coding angioplasty. Remember to always code the artery closest to the heart, but don’t forget to apply the first guideline about body parts. If the most proximal artery is in a different body system, use the general body part value in either the Upper Arteries or Lower Arteries body systems.
Step 4: Approach
The approach value is easy to misinterpret and it’s important to refer back to the official PCS approach definitions.
| Open | Definition: Cutting through the skin or mucous membrane and any other body layers necessary to expose the site of the procedure |
| Percutaneous | Definition: Entry, by puncture or minor incision, of instrumentation through the skin of mucous membrane and any other body layers necessary to reach the site of the procedure |
| Percutaneous Endoscopic | Definition: Entry, by puncture or minor incision, of instrumentation through the skin or mucous membrane and any other body layers necessary to reach and visualize the site of the procedure |
Transluminal angioplasty is performed by placing a catheter (instrumentation) into a vessel and advancing it past the lesion. The vessel can be accessed either percutaneously or via cutdown, where a small incision is made in the skin with dissection down to the vessel to be punctured. However, both procedures are coded to the approach Percutaneous because the procedural site is not exposed. The procedural site is reached with instrumentation. For example, the right femoral artery may be accessed via cutdown to perform angioplasty in the left popliteal artery. Even though the right femoral artery was exposed, the operative site is the left popliteal artery, which was not exposed. OCG B5.4 reinforces this logic:
Percutaneous procedure via device
B5.4
Procedures performed percutaneously via a device placed for the procedure are coded to the approach Percutaneous.
Example: Fragmentation of kidney stone performed via percutaneous nephrostomy is coded to the approach Percutaneous.
The approach Percutaneous Endoscopic is not used for angioplasty procedures since endoscopic visualization is not used for these procedures. The physician visualizes the arteries using fluoroscopy, a radiology modality.
Step 5: Device
While all angioplasty procedures utilize medical devices to perform the procedure (e.g., angiography and balloon catheters), the PCS definition of a device is one that remains after the procedure.
B6.1a
A device is coded only if a device remains after the procedure is completed. If no device remains, the device value No Device is coded. In limited root operations, the classification provides the qualifier values Temporary and Intraoperative, for specific procedures involving clinically significant devices, where the purpose of the device is to be utilized for a brief duration during the procedure or current inpatient stay. If a device that is intended to remain after the procedure is completed requires removal before the end of the operative episode in which it was inserted (for example, the device size is inadequate or a complication occurs), both the insertion and removal of the device should be coded.
Angioplasty alone without placement of a stent is coded as No Device (Z). If a stent was placed, device options exist for drug-eluting stents (Intraluminal Device, Drug-eluting) and bare metal stents (Intraluminal Device) as well as the number of stents placed. It is important to note that these codes are based on the number of stents placed according to type, rather than the number of vessels treated.

Step 6: Qualifier
In PCS coding, the qualifier is the “potpourri” field in code assignment. It changes depending on the type of procedure and body part/system. In the Lower Arteries body system, there is a qualifier for a drug-coated balloon (DCB). This is part of the qualifier assignment rather than the device since DCBs are used for angioplasty but are not left inside the body at the end of the procedure. If documentation does not specify that a DCB was used, the No Qualifier (Z) character is selected. The Upper Arteries Dilation table (037) does not include an option for DCB since this device is currently not FDA-approved for use in the arteries above the diaphragm.
Putting it All Together
As you begin to code an angioplasty procedure, break down the documentation and begin with step 1.
Case Example
Bob had near complete occlusion of his left external iliac artery and the lesion extended into the left common femoral artery. The right common femoral artery was percutaneously accessed and the catheter advanced to the left superficial femoral artery. Angiography confirmed the lesion. Angioplasty was performed on the bridging lesion of the left external iliac and common femoral arteries using a drug-coated balloon. Follow-up angiography showed good results.
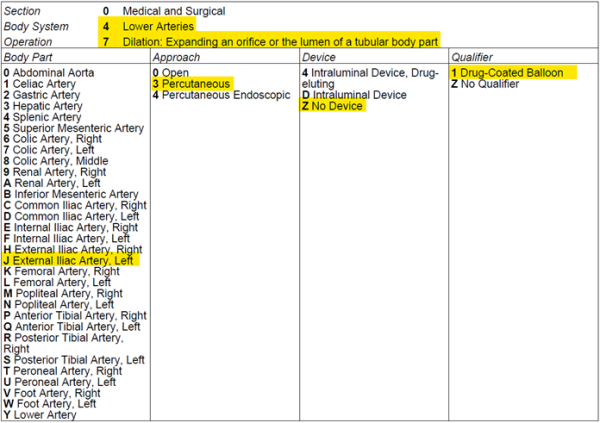
Step 1: The root operation is Dilation.
Step 2: There is a body part for the specific artery angioplastied, so this step can be skipped.
Step 3: The body part is the left external iliac artery. This is a bridging lesion from the left external iliac to the common femoral and the left external iliac artery is the most proximal vessel (OCG B4.1c). With the root operation (Dilation) and body part (left external iliac artery), the table can be selected: 047 (Dilation of Lower Arteries). The body part (fourth character) is J (External Iliac Artery, Left).

Step 4: The approach is percutaneous (3). The right common femoral artery was accessed percutaneously, and a catheter was advanced to the procedural site in the left leg.
Step 5: The device is Z (No Device). An angioplasty balloon was used, but no stents were left in place.
Step 6: The qualifier is 1 (Drug-Coated Balloon). A DCB was used during angioplasty.
The code and table selections are shown here:
047J3Z1, Dilation of Left External Iliac Artery using Drug-Coated Balloon, Percutaneous Approach
Ready for More?
Coding angioplasty procedures touches only the tip of the iceberg for vascular interventional radiology (VIR) procedures. If you want to learn more about coding VIR procedures in ICD-10-PCS, be sure to check out this month’s two-part series of on-demand webinars!

Kristi Pollard, RHIT, CCS, CPC, CIRCC, AHIMA-Approved ICD-10-CM/PCS Trainer
Senior Consultant
Kristi also performs DRG and APC audits and is known for her vast knowledge on coding vascular interventional radiology procedures. Kristi has an extensive background in coding education and consulting and is a national speakers on topics related to ICD-10 and CPT coding as well as code-based reimbursement.

You given a clear explanation about PTSA.Thank you
Thank you – great article and easy to follow when you break it down like you did. Thank you.