Q: Can diabetic foot ulcer code be used with pressure ulcers? The code book seems to indicate it would not.
A: You cannot assume a link with pressure ulcers and diabetes. Quick tip!
Q: Regarding diabetic foot ulcer. I did see the quick tip, but ICD10 indicates foot ulcer would use additional code of L97.4-L97.5--which are non-pressure. If the doctor documents the link, do we use L11.662 for other skin ulcer rather than foot ulcer--even if site is the foot?
A: If the patient has a non-pressure ulcer of a site other than foot (ankle, leg) and diabetes, you may assume a link. Use E11.622 + the code for the ulcer.
Q: So, if documentation indicated DFU but it's a pressure ulcer stage 2 of toe. Both codes can be used.
A: I would query the physician to clarify if the pressure ulcer is due to the diabetes. They need to document a link and that does not tell me the conditions are linked.
Q: If you had a doctor only document non-pressure wound, would you consider that an ulcer?
A: No, I would not. In order for it to be coded as an ulcer, they need to say ulcer somewhere in their documentation.
Q: Can you tell me if a nurse completes documentation, does the physician need to co-sign the documentation?
A: I’m assuming this means if a nurse (that is not legally responsible for establishing a diagnosis) sees the patient, can the physician co-sign the documentation so the coder and pull a diagnosis from it.
This is mentioned in a Coding Clinic dealing with malnutrition (I knew I saw it somewhere!). Take a look at Coding Clinic First Quarter 2020 page 4. The very last question asks if a physician can co-sign for a registered dietician. It specifically states the inpatient setting, but I think their answer applies to outpatient as well.
“It is beyond the scope of the Editorial Advisory Board for Coding Clinic for ICD-10-CM/PCS to address this type of documentation issue. Your hospital may develop a facility-based policy to address whether documentation that is signed-off by the patient's provider is allowed to be used for coding purposes.”
We would not consider a co-signature to be best practice. An order from the provider would be best practice.
Q: I always thought the 97597-97606 was used more by physical therapists. what does it take for a physician to bill those codes?
A: A physician can bill those codes – there is nothing that says they cannot. A physician, NPP, or therapist acting within their scope of practice and licensure may provide debridement services.
This is from CPT Assistant, August 2016, Volume 26, Issue 8, page 9 and may offer some insight:
Question: If the physician removes nonviable subcutaneous tissue using a selective, nonexcisional technique, which code should be reported: code 97597 for active wound management or code 11042 for a subcutaneous tissue debridement?
Answer: If the tissue removed is at a subcutaneous tissue level or deeper, it would be appropriate to report codes 11042-11047, depending on the deepest level of tissue removed and the total surface area of that depth removed. Multiple debridements at different depths should be added together and reported for a total surface area of each depth. However, if the tissue removed is only at the epidermis/dermis level, then it may be appropriate to report active wound care management codes (97597-97598), based on the total surface area removed.
Q: If a patient has an open wound secondary to disruption of external operation (surgical) wound, not elsewhere classified, would you code a S code for the open wound for specific site as a secondary ICD-10-CM code?
A: I would not report the open wound with 7th character “S” with the disruption of external surgical wound for 2 reasons. First, the dehiscence is not a sequela of the open wound, the open wound is actually due to the dehiscence. Second, the open wound code does not provide any additional information. It’s kind of like reporting a heart transplant status with a heart transplant complication (See the O.C.G. Section I.C.21.c.3) “Status”).
Q: I have a question on CPT 97597 and 97598. The below is the measurements that I have the question on. The right wound would be 13.2 x 6 = 78 and the left would be 11 x 4 = 44 together the wounds would be 78+44 = 122 so I would use 97597, 97598 x5. I just want to make sure that I am doing this correctly.
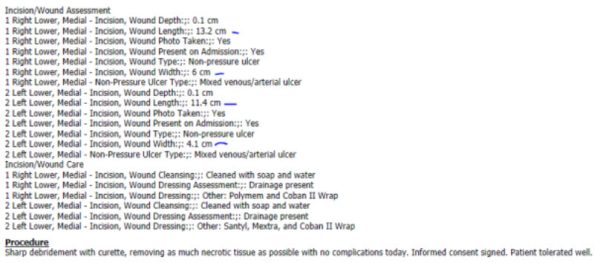
A: First, determine if these debridements are selective or excisional based on the documentation and the CPT descriptors in the book.
Yes, length x width will give you the sq cm.
For the example you provided:
R wound: 13.2 x 6 = 79.2
L wound: 11.4 x 4.1 = 46.74
If they’re both debrided the same (i.e. both selective or both excisional) add them together to get the total sq cm: 125.94. The first 20 will be reported with the initial code (97597 for selective) and the remaining measurements (105.94) with the 97598. So if these are both selective debridements that were both completely debrided (as opposed to only debriding 50% of the wound), you would report 97597 x1 and 97598 x6. Note the descriptor says “or part thereof” for the add on code.
Q: Can you code a burn based on descriptors (full-thickness, burns) or does the provider need to state the degree?
A: The O.C.G (Section I.C.19.d. Coding of Burns and Corrosions) notes " Burns are classified by depth as first degree (erythema), second degree (blistering), and third-degree (full-thickness involvement)." If you see a full-thickness burn documented, I would code that to 3rd degree.
Q: From yesterday, I would like Terri to speak to the difference between Venous Stasis I87.8 and Venous Insufficiency I87.2 Providers seem to use these terms interchangeably. Thank you.
A: I agree - they do use them interchangeably. I would recommend a conversation with them. Let them know the conditions are coded differently and create a facility guideline based on that discussion. Ideally, they should be documenting a final diagnosis. Your guidelines could instruct coders that the final diagnosis will be what you code from when there is a discrepancy.
Q: The disruption of lower leg harvest site seems it would code to disruption of surgical wound and not just T81.30xa unspecified wound.
A: I agree. The index provides the description "Dehiscence of operation wound NOS" below T81.31.
Q: How do you code a wet to dry dressing?
A: 97602. See CPT Assistant, October 2016, Volume 26, Issue 10, page 3: Wound Debridement vs. Active Wound Care Management.
Q: With the O90.0 it's not necessary to add any other ulcer code with this-correct?
A: I would not add any other codes unless they provided additional information about the patient's condition. (Per O.C.G. Section IV.A.J: Code all documented conditions that coexist).
Q: The pt. is returning for treatment of the active ulcer of toe/foot and at that point the doc says it's now healed and says return PRN. It was explained on another webinar you can use the Z51.89 with the ulcer code to indicate it's now healed. Is this not correct and I should be using the codes you've identified?
A: The Z51.89, Encounter for other specified aftercare and the instructional note states "Code also condition requiring care". Since there is no condition requiring care, I would use the Z09 code.
Q: Is the NPWT billable with both the 1104X and 97597?
A: No. Just with the 1104X debridement.
Q: If we have a nurse performing wound care if she is not certified, can we charge procedures and/or E/M levels? If so, what are the requirements we need to meet?
A: That’s typically captured by facility billing, unless it's provided incident-to in a physician-based clinic. If that’s the case, they would have to meet all the requirements for incident-to, and the E/M for nurses is 99211. This is not applicable to a hospital OP department. For procedures, we would recommend taking a look at what is allowed per state licensure.
Q: Would you put the modifier 50 on 29580 if you put the Unna boot on both feet?
A: Yes. If an Unna boot is applied bilaterally, the modifier 50 is appropriate.
Q: If the patient was seen in Wound Care for dermatitis and the dermatitis was healed. Would you code Z09 along with Z782?
A: Yes. If no other condition is being treated, Z09 and Z87.2 would be appropriate. The instructional note under Z87.2 notes it is to be used for "Conditions classifiable to L00-L99" and since dermatitis is coded with L30.9, it falls under that category.
Q: If the patient has an ulcer due to venous insufficiency and is having a debridement. I know you would typically code the venous insufficiency first and then the ulcer, but because of only debridement being billed for the date of service, would you code the ulcer and then venous insufficiency?
A: Great question! Code the venous insufficiency first, followed by the ulcer code. The fact that a debridement is being done doesn’t change the coding.
Q: Haugen indicated that we use I87.8 as the first code when a patient has venous stasis ulcer. Per 3M and the index, we think it should be I87.2. Can you please clarify?
A: Thanks for your feedback! After further review, we agree that a venous stasis ulcer (w/o varicose veins) should be reported with I87.2. Venous stasis w/o an ulcer is coded with I87.8.

Terri Reid, CCS, CCS-P, CDIP, AHIMA-Approved ICD-10-CM/PCS Trainer
Senior Coding Quality Auditor
Terri comes to Haugen Group with 20+ years of health information management experience in coding, auditing, and education. She began her career coding emergency room records and wound care records where she helped develop coding and E/M protocols and met with the providers to help them improve their documentation. Terri transitioned to an auditing role when she realized how much she enjoyed sharing her coding knowledge and experiences with other coders to help improve their skills and confidence. Terri brings her expertise in coding and auditing to the Haugen Consulting Group, having worked in previous roles leading and performing inpatient and outpatient coding audits. She is passionate about learning new medical technology and how the disease process affects illnesses.

Very interesting – can I print this?
Hi Patti – You can! If you press Control + P on your keyboard while viewing this page, it will prompt the print.
keep up the good work
good job