Is coding for shoulder procedures keeping you up at night? Don’t worry, it happens to many of us! Over the years, I have become pretty comfortable with these procedures, so I thought I would share some insights that may be helpful.
I am sure you have heard the sayings “I’ll keep that in mind” or “I’ll keep that at the back of my mind”. I like to keep my reminders like that too, but this is one that I use so frequently it stays front and center:
CMS (Centers for Medicare and Medicaid Services) considers the shoulder to be a single anatomic structure while the AAOS (American Academy of Orthopedic Surgeons) recognizes it as a complex structure.
What that means, is that when multiple shoulder procedures are performed, under the National Correct Coding Initiative (NCCI) edits used by CMS and many other payers, it would not be appropriate to add a modifier, or to bypass the edit unless the service is performed on the opposite shoulder.
Because of these different views, coding shoulder surgeries can be somewhat challenging. Let’s take a look at the terms and codes to be familiar with when coding shoulder procedures.
Arthroscopic vs. Open
During an arthroscopic repair, a surgeon creates several small incisions, usually referred to as portals. The documentation will usually mention a small camera, called an arthroscope, which is inserted into the shoulder joint. The surgeon will usually use multiple portals to gain access to different structures in the shoulder area.
An open approach is typically required for those repairs that are more complex and those that are not amenable to the arthroscopic approach. These involve incisions and direct visualization for the structure being repaired.
There is also a “mini-open” rotator cuff repair that is frequently used. These are coded and reported as an open technique per CPT. There are two code options, one for acute and one for chronic, therefore it’s important for the provider to appropriately document the diagnosis in the report in order to capture the correct CPT. If the terms acute or chronic are not specified in the operative report, coders could potentially check the patient’s history for additional information that could help identify whether the condition is due to an injury, trauma or of a degenerative nature. If all else fails, query the provider. Keep in mind though, operative reports “should be” considered as “stand alone” documents.
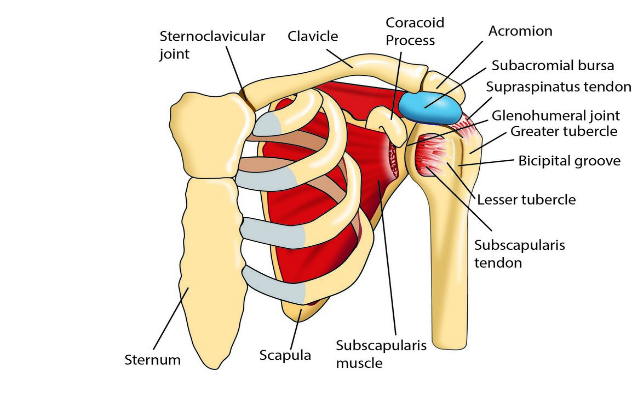
Rotator cuff anatomy
To accurately code for rotator cuff repairs, you should have a good understanding of the shoulder anatomy. The rotator cuff itself consists of four tendons: Supraspinatus, Infraspinatus, Teres Minor and Subscapularis.
When it comes to coding for a rotator cuff repair, only one code can be reported - even if they repair more than one tendon. For instance, if they do a repair on both the supraspinatus and the teres minor tendons, we can still only report it as one rotator cuff repair.
Superior Labrum from Anterior to Posterior (SLAP) Repairs
Providers should be documenting the type of SLAP tear to help us get to the right code. Here are the four types.
- Type I: Labral fraying with firmly attached labrum and biceps origin
- Type II: Labrum and biceps origin are detached from the labrum
- Type III: Bucket-handle labral tear with firmly attached labrum and biceps origin
- Type IV: Bucket-handle tear of the superior labrum with extension into the biceps tendon with biceps displacement.
The Type I and Type III SLAP are coded as limited debridement. Both the labrum and the biceps are still attached.
The other two types, Types II and IV, involve disruption of the labrum attachment and should be reported using code 29807 (arthroscopic) to indicate repair of the lesions.
Subacromial Decompression with Partial Acromioplasty (29826)
Keep in mind that CPT 29826 is an add-on code and requires a primary procedure code. It also requires both a subacromial decompression and a partial acromioplasty. If an acromioplasty is not performed, report only a debridement.
When coding for an acromioplasty, look for documentation about the morphology (specifically type I, II, or III) in the operative notes. The documentation should also show that change was made to the anatomy. Removing osteophytes is not considered an acromioplasty and should be reported as a debridement.
Also, if the provider documents only that a subacromial bursectomy was performed, this does not qualify for this code. A bursectomy would be considered a limited debridement (29822) since this is soft tissue only. Its super important to watch the documentation!
Distal Claviculectomy (29824)
This one is easy to code (or so I think). Documentation should consist of 1 cm of the distal clavicle being removed. Anything less than that would be a debridement (29822/29823). Reference: AMA CPT® Changes: An Insider’s View 2002 and AAOS “April 2004 Bulletin”.
Debridements (29822/29823)
Regarding the difference between 29822 and 29823, most payers, including CMS, follow AAOS guidelines, which state extensive debridement includes debridement of multiple soft structures, multiple hard structures, or a combination of both.
If the surgeon is debriding a rotator cuff tear and then repairing, you won’t be able to capture a debridement. So, what this means is that if the surgeon is cleaning up or debriding one of the muscles of the rotator cuff and then goes on to repair it, you cannot count this towards a debridement code. The debridement is considered inclusive of the rotator cuff repair.
In the end, its all about the anatomy, documentation and guidelines and putting the puzzle pieces together to get that final picture.

Mary Bort, CPC, CPMA, CANPC, CASCC, COSC
Consultant
Mary is a consultant for The Haugen Consulting Group with over 25 years of health care industry experience. She started her career in Orthopedics which was her passion for decades. In addition to Orthopedics, she provides expertise in other specialties such as Anesthesia, Ambulatory Surgery Center, as well as most surgical specialties . She has experience working the professional fee side of coding, audit, education as well as compliance, serving both coders and physicians, as well as the surgical side. She is a Certified Professional Coder (CPC), Certified Professional Medical Auditor (CPMA), Certified Anesthesia Professional Coder (CANPC) Certified Ambulatory Surgery Center Coder (CASCC) and Certified Orthopedic Surgery Coder (COSC).
During her free time, she loves to do crafts, enjoys the outdoors, and the Broncos! She has 4 daughters, and 10 grandchildren which light up her life.

Hi can we have the original pdf shared by AMA on Distal Claviculetomy for AMA CPT® Changes: An Insider’s View 2002
Hi Sharanya,
Unfortunately, due to copyright laws, we are unable to provide copies of AMA literature.
Does multiple procedure reduction apply to add-on codes like 29826?
Hi Lisa, Procedure codes identified as “add-on” codes are not subject to multiple surgical procedure reductions. Thank you!
NCCI policy states that ” “If an arthroscopic procedure is converted to an open procedure, only the open procedure may be reported” Are we allowed to bill arthroscopic code like 29823 combined with open Biceps tenodesis?
Hi Andrea,
If the debridement is done arthroscopically on other distinct structures, (not the biceps) — then yes you can separately report an arthroscopic debridement in addition to an open code. The AMA has new guidance/recommendations that address open vs scope. Mary also discusses your scenario type as well as the new guidance in her recent “Procedure Coding for Joint Injections & Arthroscopies” webinar. https://www.thehaugengroup.com/marketplace/webinars/2023/procedure-coding-for-joint-injections-arthroscopies/
Hi Mary – I have a tricky situation where the providers are documenting a perfect 29826 but prefer to bill 29823, which is applicable if we use the bursectomy and acromial debridement (to level 1) as sites of 29823. Is there anything that says we have to bill 29826?
Hi Natalie!
Here is the reply from our team:
Based on what you describe, this does not appear to qualify for 29823. If they are performing a bursectomy and changing the anatomy of the acromion, then 29826 should be coded.